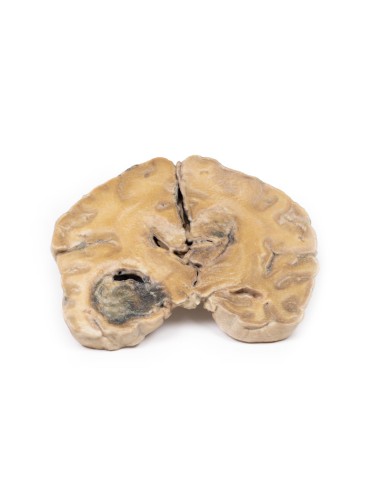
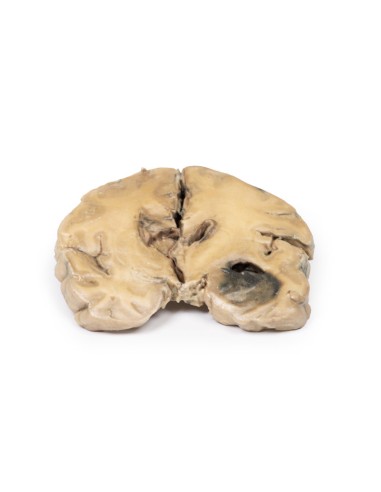
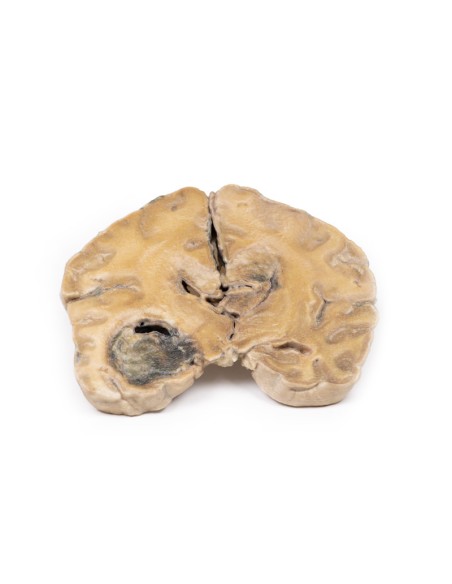
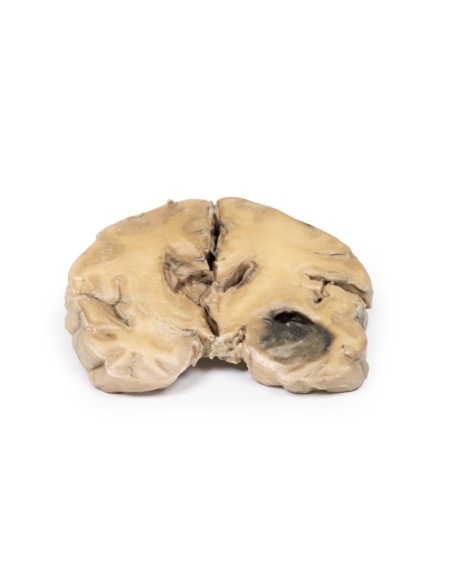
Glioblastoma multiforme - Erler Zimmer 3D anatomy Series MP2015
erler zimmerMade in ultra-high resolution 3D printing in full color.
Glioblastoma multiforme - Erler Zimmer 3D anatomy Series MP2015
This dissection model highlighting a Glioblastoma multiforme is part of the exclusive Monash 3D anatomy series, a comprehensive series of human dissections reproduced with ultra-high resolution color 3D printing.
Clinical history
Over a 3-year period, a 57-year-old woman had intermittent frontal headache and memory disturbances with progression to psychiatric disorders and finally vomiting and meningeal signs. Neurological signs of localization developed only late in the course of the disease.
Pathology
Coronal section of the cerebral hemisphere shows a round, hemorrhagic, variegated tumor in the left temporal lobe. Less well-defined tumor tissue extends along the midline replacing the corpus callosum. The ventricular system has been almost completely obliterated. Further sections of the cerebral hemisphere confirmed that these apparently separate lesions are extensions of a massive tumor.
Further information
Gliomas are the second most common tumor of the central nervous system after meningiomas. The term "glioma" refers to tumors that are histologically similar to normal glial (macroglial)* cells, i.e., astrocytes, oligodendrocytes and ependymal cells. They arise from a progenitor cell that differentiates one of the cell lines. GBMs can arise in the brain "de novo" or evolve from lower grade astrocytomas or oligodendrogliomas. GBM are often referred to as grade IV astrocytomas. They differ histologically from anaplastic astrocytomas by necrotizing tissue surrounded by anaplastic cells and the presence of hyperplastic blood vessels.
GBMs are more common in males. It is most commonly diagnosed in the sixth decade of life. Genetic risk factors include neurofibromatosis type 1 and Li-Fraumeni syndrome. Previous brain radiation therapy is also associated with an increased risk of GBM. Symptoms vary depending on the location of the GBM, but may include any of the following:
- Persistent headache
- Double or blurred vision
- Vomiting
- Loss of appetite
- Changes in mood and personality
- Changes in ability to think and learn
- New onset of seizures
- Speech difficulties with gradual onset
Diagnostic tools include computed tomography (CT) and magnetic resonance imaging (MRI). About 50% of these tumors occupy more than one cerebral hemisphere. GBMs commonly extend into the ventricular walls or meninges and then into the central spinal fluid (CSF). Spinal cord spread is rare. Metastasis beyond the central nervous system is rare. Tumor growth causes cerebral edema leading to increased intracranial pressure. These are biologically aggressive tumors, and if left untreated, survival is typically 3 months. The mainstay of treatment for GBM is surgery, followed by radiation and chemotherapy.
*Microglia are a different strain from macroglia. The former are related to the macrophage lineage and are derived initially from the yolk sac and later in development from the bone marrow.
What advantages does the Monash University anatomical dissection collection offer over plastic models or plastinated human specimens?
- Each body replica has been carefully created from selected patient X-ray data or human cadaver specimens selected by a highly trained team of anatomists at the Monash University Center for Human Anatomy Education to illustrate a range of clinically important areas of anatomy with a quality and fidelity that cannot be achieved with conventional anatomical models-this is real anatomy, not stylized anatomy.
- Each body replica has been rigorously checked by a team of highly trained anatomists at the Center for Human Anatomy Education, Monash University, to ensure the anatomical accuracy of the final product.
- The body replicas are not real human tissue and therefore not subject to any barriers of transportation, import, or use in educational facilities that do not hold an anatomy license. The Monash 3D Anatomy dissection series avoids these and other ethical issues that are raised when dealing with plastinated human remains.